PFO Closure ‘The Thing to Do’
Closure of patent foramen ovale (PFO) may alleviate decompression sickness. Serious divers should seek screening, says doctor.
Small study looks at divers who simulated deep dives in hyperbaric chamber. Arterial bubbles was detected in 12% of divers with PFOs and 0% with closed PFOs.
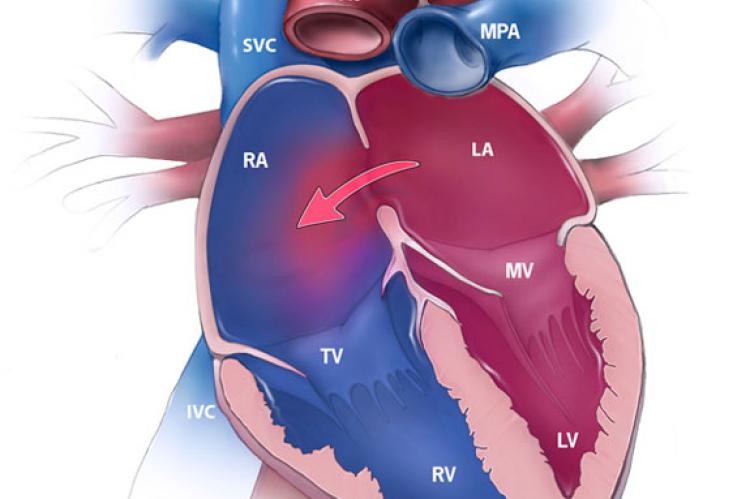
Atrial septal defect (ASD) is a form of a congenital heart defect, such as a hole, that enables blood flow between two compartments of the heart called the left and right atria; Oxygen-rich blood can flow directly from the left side of the heart to mix with the oxygen-poor blood in the right side of the heart, or vice versa.
What is PFO?
During fetal development a hole in the septum called the foramen ovaleallows blood from the right atrium to enter the left atrium . This opening allows blood to bypass the nonfunctional fetal lungs while the fetus obtains its oxygen from the placenta.
After birth, in approximately 25% of adults the foramen ovale does not entirely seal.
In some cases elevation of the pressure in the pulmonary circulatory system can cause the foramen ovale to remain open. This is known as a patent foramen ovale (PFO)
What is the significance for divers?
In many cases an ASD may not produce noticeable signs or symptoms, especially if the defect is small. However ASDs, and particularly PFOs, are a predisposing risk factor for decompression sickness in divers because a proportion of venous blood carrying inert gases, such as helium or nitrogen does not pass through the lungs.[26][27] The only way to release the excess inert gases from the body is to pass the blood carrying the inert gases through the lungs to be exhaled. If some of the inert gas-laden blood passes through the PFO, it avoids the lungs and the inert gas is more likely to form large bubbles in the arterial blood stream causing decompression sickness.
Test
Czech medical reseachers simulated dives in a hyperbaric chamber of either 18 m for 80 min or 50 m for 20 min. 'Divers' were categorized according to whether they had a PFO or not. On echocardiography, venous bubbles were detected in both groups with equal frequency.
Findings
However, arterial bubbles were detected in 12% of the PFO group but none of the closure patients. Furthermore, In 21% of divers with PFO and detected arterial gas bubbles, neurological symptoms of decompression sickness were present (ie, headache, unusual fatigue, and transitory visual disturbances). Conversely, none of the divers in the closure group reported decompression sickness symptoms.
Implications
The data should convince serious divers to seek screening for the presence of a PFO. Robert J. Sommer, MD, of Columbia University Medical Center stated in an interview with TCTMD.
Dr. Sommer notes that he has seen professional divers from organizations such as the New York Police Department and the New York Fire Department who have experienced symptoms on the job and subsequently been found to have a PFO. “And then those patients come to me to get their PFOs closed because otherwise they would be classified as disabled,” and would not be allowed to dive again, he said